Diabetic neuropathy is a type of nerve damage that can occur in individuals with diabetes. This condition arises when high blood sugar levels over time lead to damage in the peripheral nerves, which are responsible for transmitting signals between the brain and the rest of the body. As a result, you may experience a range of symptoms that can affect your quality of life.
The condition can manifest in various forms, impacting different parts of the body, and it often develops gradually, making it easy to overlook in its early stages. Understanding diabetic neuropathy is crucial for anyone living with diabetes. It is not just a single disorder but rather a group of related conditions that can affect your sensory, motor, and autonomic nerves.
Sensory neuropathy may cause pain or numbness in your extremities, while motor neuropathy can lead to muscle weakness and coordination issues. Autonomic neuropathy affects involuntary bodily functions, such as digestion and heart rate. Recognizing the signs and symptoms early on can help you manage the condition more effectively and maintain a better quality of life.
Common Symptoms of Diabetic Neuropathy
The symptoms of diabetic neuropathy can vary widely depending on the type of nerves affected. One of the most common signs is a tingling or burning sensation in your hands and feet. You might also experience sharp pains or increased sensitivity to touch, which can make everyday activities uncomfortable.
As the condition progresses, you may notice a loss of sensation, making it difficult to feel temperature changes or even minor injuries, which can lead to complications if left untreated. In addition to sensory symptoms, you may also encounter motor symptoms that affect your ability to move and coordinate your body. Weakness in your muscles can make it challenging to perform tasks that require fine motor skills, such as buttoning a shirt or holding a pen.
Furthermore, autonomic neuropathy can lead to symptoms like dizziness when standing up, digestive issues such as nausea or bloating, and even problems with sexual function. These diverse symptoms can significantly impact your daily life, making it essential to seek medical advice if you suspect you may be experiencing diabetic neuropathy.
Types of Diabetic Neuropathy
Diabetic neuropathy is categorized into several types based on the nerves affected. The most common form is peripheral neuropathy, which primarily impacts the legs and feet. This type often leads to pain, tingling, and numbness in these areas, making it difficult for you to walk or maintain balance.
If you find yourself frequently tripping or experiencing foot injuries without realizing it, peripheral neuropathy could be the culprit. Another type is autonomic neuropathy, which affects the nerves that control involuntary bodily functions. This can lead to issues such as abnormal heart rates, digestive problems, and difficulties with sweating.
You might notice that your body does not respond as it should in certain situations, such as feeling excessively hot or cold. Additionally, focal neuropathy is another form that affects specific nerves, often leading to sudden weakness or pain in one area of the body, such as the eyes or face. Understanding these different types can help you identify your symptoms more accurately and communicate effectively with your healthcare provider.
Risk Factors for Diabetic Neuropathy
Several risk factors contribute to the development of diabetic neuropathy, and being aware of them can empower you to take proactive steps in managing your health. One of the most significant risk factors is prolonged exposure to high blood sugar levels. If you have difficulty controlling your blood glucose levels over time, your chances of developing nerve damage increase substantially.
Therefore, maintaining stable blood sugar levels through diet, exercise, and medication is crucial. Other risk factors include the duration of diabetes; the longer you have had diabetes, the higher your risk for neuropathy. Additionally, factors such as high blood pressure, high cholesterol levels, smoking, and obesity can exacerbate nerve damage.
If you have a family history of diabetes or neuropathy, you may also be at an increased risk. By understanding these risk factors, you can work with your healthcare team to create a personalized plan that addresses your unique situation and helps mitigate potential complications.
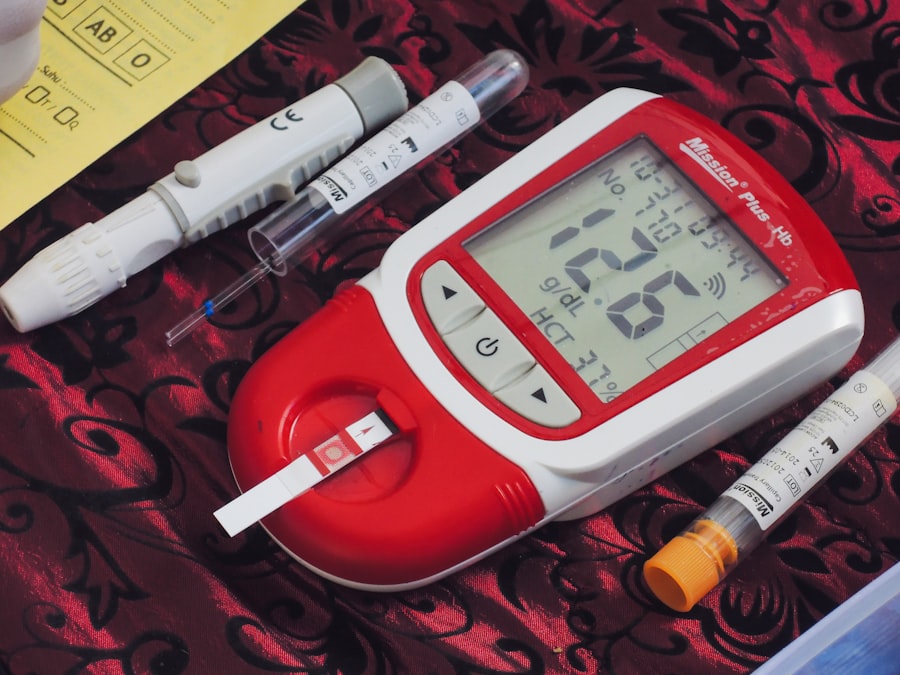
Diagnosing Diabetic Neuropathy
Diagnosing diabetic neuropathy typically involves a combination of medical history assessment, physical examinations, and specific tests to evaluate nerve function. Your healthcare provider will likely begin by asking about your symptoms and how long you’ve been experiencing them. They may also inquire about your diabetes management history and any other health conditions that could contribute to nerve damage.
During the physical examination, your doctor may perform various tests to assess your reflexes, muscle strength, and sensory responses. For instance, they might use a tuning fork or monofilament test to check for sensitivity in your feet. In some cases, additional tests such as nerve conduction studies or electromyography (EMG) may be necessary to measure how well electrical signals travel through your nerves.
These diagnostic tools help determine the extent of nerve damage and guide appropriate treatment options tailored to your needs.
Treatment Options for Diabetic Neuropathy
While there is currently no cure for diabetic neuropathy, several treatment options can help manage symptoms and improve your quality of life. One of the primary goals is to control blood sugar levels effectively. By maintaining stable glucose levels through diet, exercise, and medication adherence, you can slow the progression of nerve damage and alleviate some symptoms.
In addition to blood sugar management, various medications may be prescribed to help relieve pain associated with diabetic neuropathy. Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may provide some relief for mild discomfort. For more severe pain, your doctor might recommend prescription medications such as antidepressants or anticonvulsants that have been shown to be effective in managing nerve pain.
Physical therapy can also play a vital role in improving mobility and strength while reducing discomfort.
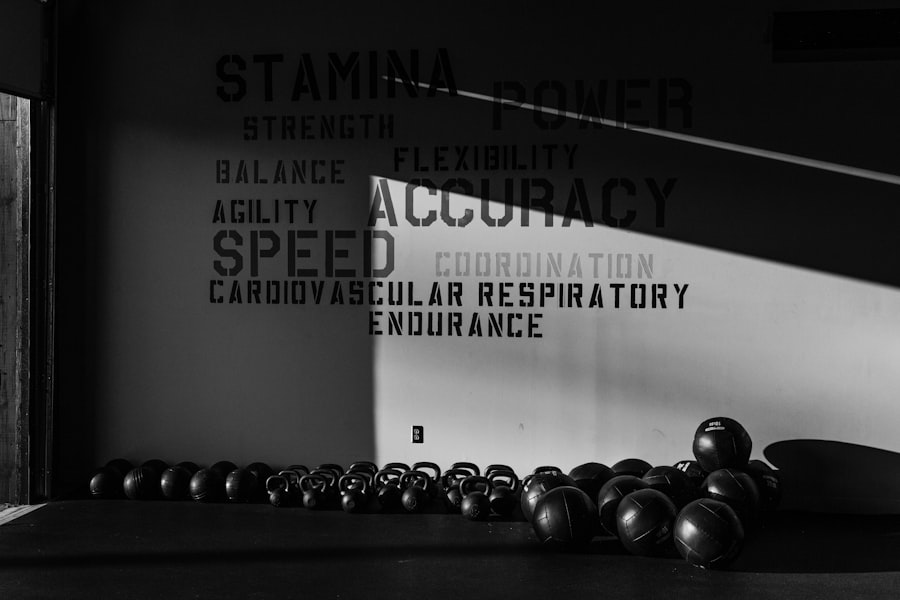
Preventing Diabetic Neuropathy
Preventing diabetic neuropathy largely revolves around effective diabetes management and lifestyle choices. One of the most critical steps you can take is to monitor your blood sugar levels regularly and work closely with your healthcare team to develop a personalized management plan. This plan should include dietary modifications that focus on whole foods while limiting processed sugars and carbohydrates.
In addition to blood sugar control, adopting a healthy lifestyle can significantly reduce your risk of developing diabetic neuropathy. Regular physical activity is essential; aim for at least 150 minutes of moderate exercise each week. This not only helps regulate blood sugar levels but also improves circulation and overall nerve health.
Furthermore, avoiding smoking and limiting alcohol consumption can contribute positively to your nerve health. By making these proactive choices, you can significantly lower your risk of developing diabetic neuropathy.
Living with Diabetic Neuropathy: Tips and Support
Living with diabetic neuropathy can be challenging, but there are numerous strategies you can employ to manage your symptoms effectively. One essential tip is to stay informed about your condition; understanding diabetic neuropathy will empower you to make better decisions regarding your health care and lifestyle choices. Joining support groups or online communities can also provide valuable emotional support from others who share similar experiences.
Incorporating self-care practices into your daily routine is crucial for managing symptoms effectively. Regular foot care is particularly important; inspect your feet daily for any cuts or sores that may go unnoticed due to reduced sensation. Wearing comfortable shoes that fit well can help prevent injuries as well.
Additionally, practicing stress-reduction techniques such as mindfulness or yoga can improve both mental well-being and physical health. By taking these steps and seeking support when needed, you can navigate life with diabetic neuropathy more confidently and maintain a fulfilling lifestyle despite the challenges it presents.